It's been about 9 months since I've written anything partly due to the sheer exhaustion of job hunting and partly due to the nuances of working full time as a night nurse...it took about a month and half after passing boards, but I landed a job, thank God (which by today's labor market for new grads, was lightening fast!)
Acute medical surgical telemetry...which means you get it all. Sick, sicker and sickest. Sepsis, pneumonia, post ops, chest pain, GI bleeds, MRSA wounds, vacs, UTIs, psych, dementia, DTs, knees, hips, pelvis, abdominal this and that, and an occasional prolapsed anything. Atrial fibrillation, PVCs, bigeminy and an occasional third degree block. This is the menu on my unit and there is always something new. In nine months, I have only seen one patient who had a family member present at the time of death. Every other patient died alone, except for their nurse who is always present.
Working nights, I have lost contact with a lot of my daytime friends and family. This is the only drawback, otherwise I have adapted to the changes in sleep, because my family has made the adjustment with me. We have a do not disturb button on our house phone and since all of us have cell phones now, we don't miss the ringer on the house phone. When I started working noc shift, I marveled at my co-workers ability to eat anything in the middle of the night, but within 3 weeks, my body clock shifted and I found myself famished at 0200. I usually wake up at 1600-1700 without any breakfast pangs and then force myself to eat something before 1900. By 0200, I am hungry. I eat one more time..usually at 0800-0900 and that is it for my work day. I eat twice per day. As a result, I lost about 20 pounds since starting work. It is so strange what your body does to compensate for the shift change. I wake up in the middle of the afternoon after working all night and the first feeling of disorientation is so strange (i.e. where am I, what time of day - should be morning but my brain realizes it is late afternoon, early evening) Some days, after working three 12 hour shifts in a row or an occasional 16 hr shift, I will wake up at 2100 (9 PM) and stay up all night. It's the most surreal feeling to live and work like this when your family lives on an opposite pole. I noticed during the holidays, everybody shifted to my schedule and stayed up later and slept later...so we could spend more time together.
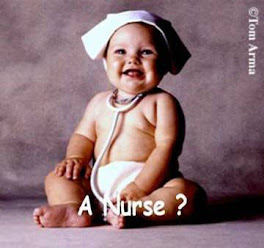
I can say with certainty that I have no regrets about becoming a nurse. It is the hardest, most rewarding career. Everyday is different. After 9 months of labor, I still feel like a baby. I have wonderful colleagues who teach me something new all the time...it's a wild ride worth taking..and I hope I still feel this way 5 years from now.